
Animal Rabies diagnosis & Research laboratory
Animal Rabies diagnosis & Research laboratory
Epidemiology & Infection
Epidemiology

Rabies is a zoonosis which continues to spread.. It is one of the oldest diseases known to man. During the past seven centuries, the many published reports indicate the almost global presence of the disease. Most countries now report either canine rabies, which frequently leads to death in humans, or wildlife rabies, which spills-over into domestic animals; some countries report both forms of the disease. With the exception of the Scandinavian Peninsula and a few island countries such as Japan ,New Zealand and great Britain.
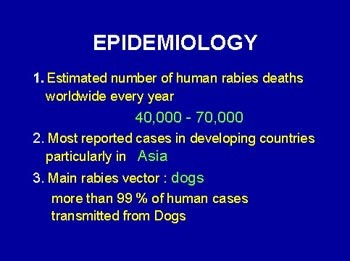
The number of deaths caused each year by rabies is estimated to be at least 50000 worldwide. Most human cases are reported from developing countries, particularly the Indian sub-continent, where canine rabies is virtually out of control.An estimated more than 10 million people recieive post - exposure treatments each year after being exposed to rabies suspect animals.
The number of rabies cases in animals has been reduced in European countries that have conducted campaigns to orally immunize wildlife. Dramatic decreases in human cases of rabies have also been reported during recent year in Thailand folowing implementation of programmes for improved post - exposure treatment of humans.
In developed countries , rabies is today found mainly in wild animal hosts, from which the disease spills over to domestic animals and humans.
By contrast,in most countries of Africa, Asia and Latin America dogs continue to be the main hosts and are responsible for most of the rabies deaths that occur worldwide.
The most frequent ways that humans becom infected with rabies is through the bite of infected dogs and cats,wild carnivorous species like foxes,raccoons, skunks, wolves and vampire bats. Cattle ,horses,and other herbivores can become infected with rabies but rarely transmit the virus to other animals, althought they may transmit the disease to human.
There have been reported cases of human - to - human rabies transmission by corneal transplants. These cases underscore the importance of not using transplant tissue from anyone who died of a neurologic illness of unknown cause.
Infection
Rabies is spread via virus in the saliva of an infected animal which bites a susceptible host. The virus is neurotropic but may replicate in muscle fibres before invading the nervous system. Once virus has entered the peripheral nerves it is passed to the central nervous system (CNS) by retrograde axoplasmic transport.
Virus spread within the brain
Within the brain, virus spreads from infected to contiguous cells. There may be regional differences in the intensity with which areas of the brain become infected. The main areas affected are usually the cerebellum, hypothalamus, hippocampus.
Virus spread from the brain
Virus moves centrifugally from neural perikarya in the CNS and cerebrospinal ganglia, to affect almost all nerves of the body. As a result, many non-neural cells, including cells of the salivary glands, become infected and infectious virus may occur in saliva before the onset of clinical disease.
Infection of salivary glands
Virus may be present in the saliva for many days before clinical signs appear and it may be steadily or intermittently secreted until just before death.

Incubation
Factors which may influence the length of the incubation period include the site of the bite, the amount of virus in the saliva of the biting animal, the virus strain, and the age and immune status of the victim. The incubation period in naturally infected animals is not well documented but is known to be very variable, from a few days to several months. Early signs in dogs last 2–5 days and in 80 % of cases then progress to furious and 20 % to the dumb form in the remainder. Paralysis and death occurs in both dumb and furious forms 4– 8 days after the onset of clinical signs.
The incubation period in humans is also very variable and may last from 2 weeks to as long as 6 years. Patients with the furious form of the disease generally die rapidly within 7 days after clinical onset, though survival may be as long as 2–3 weeks in paralytic cases.
Virus excretion in animals
Virus may be present in the saliva for many days before clinical signs appear and it may be steadily or intermittently.


